The Path to Becoming a Podiatrist
Podiatrists are physicians and surgeons who specialize in the diagnosis and treatment of conditions and injuries of the foot, ankle, and lower leg. Becoming a podiatrist requires extensive education. Aspiring podiatrists first get a bachelor’s degree which is usually focused on biology, chemistry, and anatomy, along with the necessary prerequisites for attending an accredited medical school, where they will graduate with a Doctorate of Podiatric Medicine (DPM). This is followed by a medical and surgical residency at an approved health care facility. Some podiatrists continue their education with a post-graduate fellowship. To become a licensed podiatrist in the United States, the doctor must pass the American Podiatric Medical Licensing Examination. Additionally, podiatrists may opt to become board certified with certain organizations, including the American Board of Podiatric Medicine (ABPM). Podiatrists usually engage in continuing medical education to maintain their license to practice and to stay abreast of industry trends.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Nrup Tolat, DPM from Atlanta Total Foot & Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
- Diagnose foot ailments such as ulcers, tumors, fractures, etc.
- Use innovative methods to treat conditions
- Use corrective orthotics, casts, and strappings to correct deformities
- Correct walking patterns and balance
- Provide individual consultations to patients
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
What Is Diabetic Peripheral Neuropathy?
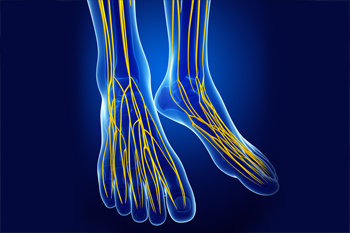
People with diabetes are at an increased risk of neuropathy, or nerve damage. Diabetics are frequently diagnosed with peripheral neuropathy, or nerve damage in the hands and feet. Symptoms of peripheral neuropathy in the lower limbs include tingling, pins and needles, numbness, pain, or increased sensitivity in the feet. In some cases, the feet may change shape due to nerve damage. Sores and diabetic foot ulcers, which can be difficult to detect and tend to heal slowly and poorly, are also very common. If you have diabetes, it is important to be vigilant of any foot or ankle symptoms. Seeing a podiatrist regularly can help manage existing symptoms, detect and treat any new problems, and maintain the health of your feet.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Nrup Tolat, DPM from Atlanta Total Foot & Ankle Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
What Can Cause Heel Pain?
 Heel pain can be debilitating for some patients, and can arise due to a variety of different causes. The three most common sources of heel pain are plantar fasciitis, Achilles tendonitis, and arthritis. Plantar fasciitis occurs when the plantar fascia, which is a band of tissue that runs along the bottom of the foot connecting the heel to the toes, becomes inflamed or torn. Achilles tendonitis is the result of the Achilles tendon, which connects the calf muscles to the heel bone, becoming inflamed. Other common causes of heel pain can include bursitis, stress fractures, or the wearing down of the heel pad at the bottom of the heel. If you are struggling with heel pain, consulting with a podiatrist for a proper diagnosis and treatment can be incredibly beneficial.
Heel pain can be debilitating for some patients, and can arise due to a variety of different causes. The three most common sources of heel pain are plantar fasciitis, Achilles tendonitis, and arthritis. Plantar fasciitis occurs when the plantar fascia, which is a band of tissue that runs along the bottom of the foot connecting the heel to the toes, becomes inflamed or torn. Achilles tendonitis is the result of the Achilles tendon, which connects the calf muscles to the heel bone, becoming inflamed. Other common causes of heel pain can include bursitis, stress fractures, or the wearing down of the heel pad at the bottom of the heel. If you are struggling with heel pain, consulting with a podiatrist for a proper diagnosis and treatment can be incredibly beneficial.
Many people suffer from bouts of heel pain. For more information, contact Nrup Tolat, DPM of Atlanta Total Foot & Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
Tarsal Tunnel Syndrome Causes
The tarsal tunnel is a narrow space in the inner ankle that has nerves, blood vessels, and tendons passing through it. When the posterior tibial nerve inside of the tarsal tunnel is compressed, this leads to a painful condition called tarsal tunnel syndrome. Symptoms of this condition include foot pain, a pins and needles sensation, numbness, and swelling. The nerve compression that brings about tarsal tunnel syndrome can be caused by sports injuries, lesions, such as ganglion cysts, that occupy space in the tunnel, excess fluid buildup, changes in the biomechanics of the foot, wearing tight, ill-fitting shoes, or other medical conditions like diabetes and arthritis. In about 30% of cases, the cause is unknown. Nevertheless, tarsal tunnel syndrome can be treated and usually resolves within several weeks of treatment. If you have symptoms of this condition, please seek the care of a podiatrist.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Nrup Tolat, DPM of Atlanta Total Foot & Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
Foot Care for Dry, Cracked Heels
Dry, cracked heels can be annoying to deal with on a daily basis. They can even be painful when left untreated. Cracked heels are often caused by a lack of moisture and this can result from cold winter weather, dehydration, exposing your feet to hot water for prolonged periods of time, or scrubbing your feet while they are dry. Certain skin conditions, such as eczema and psoriasis, can also make the heels very dry. Having a good foot care regiment at home can help alleviate dry, cracked heels. Your foot care routine may include soaking the feet in warm water, exfoliating the heels with a pumice stone, thoroughly drying your feet with a towel, and then applying a heavy moisturizing cream. If the cracks on your heels become so deep that they bleed, these are known as fissures and can lead to an infection. When your cracked heels are painful, bleeding, or if you have diabetes, it is strongly suggested that you see a podiatrist for treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Nrup Tolat, DPM from Atlanta Total Foot & Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Woodstock and Atlanta, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.